Whether you are vaccinated or not, being up to date with Cervical Screening remains the most important protection against cervical cancer. In Australia, since 1991, Australian women and people with a cervix have been able to participate in cervical screening through the National Cervical Screening Program.
In 2017, the Pap test (or Pap smear) has been replaced by the HPV test, or Cervical Screening Test (also referred to as CST). This better technology helps improve early detection of cervical cancer and save lives and is scheduled every 5 years (instead of every 2 years for the old Pap Test).
The new Cervical Screening Test detects whether human papillomavirus (HPV) is present and has proven very effective at early detection.
The current guidelines recommend that every woman and person with a cervix from the ages of 25-74 who has ever had sexual contact, should have a Cervical Screening Test every five years
even if you have:
There are now two options for your next Cervical Screening Test.
You can choose to have a healthcare provider do the test or you can choose to self-collect your test, using a small swab. For many, self-collection is a less daunting and more comfortable option.
Both testing options are available through a healthcare provider and are equally as accurate at detecting HPV, which causes almost all cases of cervical cancer.

Have your doctor or nurse perform a cervical screening test (Download the cervical screening Comfort Checklist to ensure this method is as comfortable as possible).

Self-Collection – talk to your doctor or nurse about choosing to collect your sample yourself.
Your doctor or nurse will take a sample from your cervix in a health clinic. A speculum will be inserted into your vagina to view your cervix. They will then collect a sample of cells from your cervix with a small brush.
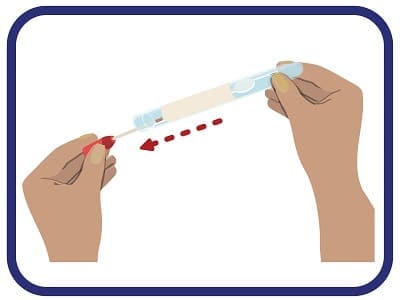
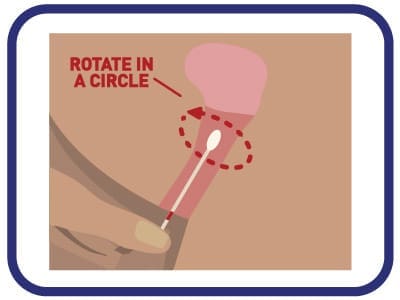
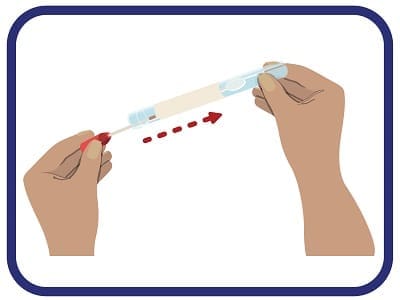
Self-collection enables you to collect your own cervical screening test sample from your vagina using a small swab. It’s quick, easy, private, and just as accurate as detecting HPV as a test done by your doctor or nurse. Your doctor or nurse will give you a small swab, explain how to do the test and direct you to a private space in the clinic
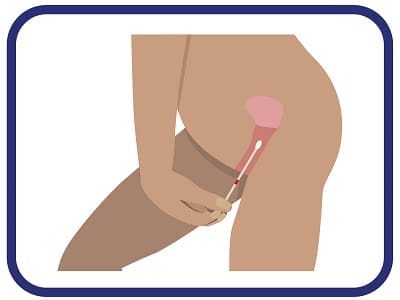
Tip: It may be easier to use your other hand to hold the outer skin at the entrance of your vagina
Depending on the result (for either testing option), you may need to have another Cervical Screening Test in
12 months to see if the HPV infection has cleared or you might be referred to a specialist for a colposcopy.
A colposcopy is a procedure that takes a closer look at the cells of the cervix.
The Comfort Checklist is a tool to help you prepare for your cervical screening test so you can have a positive screening experience. Developed by ACCF and a panel of experts. The Comfort Checklist is designed to overcome some of the barriers that prevent some women and people with a cervix from participating in preventive screening.
One third of Australians are not participating in cervical screening as frequently as recommended. This means they are overdue or have never presented for screening. If we want to see cervical cancer eliminated by 2035, we need these cervical screening numbers to rise.
Please share this resource with your friends to help increase cervical screening rates.
The Cervical Screening Test (CST) introduced in 2017 is more effective at detecting the human papillomavirus (HPV) that causes cervical abnormalities, at an earlier stage. Prior to 2017, the Pap test (or Pap smear) was utilised. It looked for cell changes in the cervix, whereas the Cervical Screening Test looks for the human papillomavirus (HPV) which can lead to cell changes in the cervix.
Cervical cancer is rare, and it usually takes 10 years for abnormalities caused by HPV to develop into cervical cancer. The new CST is a more accurate, effective and safe test to have every five years instead of the two-yearly Pap test.
Aggressive, fast-growing cancers are very rare and usually diagnosed when women see a doctor after noticing symptoms. All screening programs are designed for women without symptoms.
Women of any age who have symptoms (including pain or abnormal vaginal bleeding or discharge) should see their doctor immediately.
The Cervical Screening Test (CST) detects human papillomavirus (HPV) infection, which is the first step in developing cervical cancer. Persistent HPV infections can cause abnormal cell changes that may lead to cervical cancer. However, this usually takes a long time, often more than 10 years from initial HPV infection. While the old Pap test (or Pap smear) could detect abnormal cell changes, the Cervical Screening Test will detect the persistent HPV infection that causes the abnormal cell changes, prior to the development of cancer.
If you choose for your health practitioner to conduct the screening, the procedure for collecting the sample for HPV testing is the same as the procedure for having a Pap smear. A doctor or nurse takes a small sample of cells from the woman’s cervix.
If you choose self-collection, you will be given a self-collection kit and instructed on how to collect cells from your vagina. The samples collected are then sent away to a laboratory to be examined.
A self-collected sample is taken from the vagina and is checked for human papillomavirus (HPV). You will need to visit your doctor or nurse to get the kit and will then take your sample in a private space, such as a bathroom. All you need to do is insert a swab a few centimetres into your vagina and rotate it for 20 to 30 seconds. Learn how to take your own sample and find more information at Self-collection for the Cervical Screening Test.
To make an appointment with a health professional to have a Cervical Screening Test, you can contact:
A Cervical Screening Test (CST) is a relatively simple procedure that only takes a few minutes and should not be painful. Your screening experience should include:
Your GP or health professional should let you know if you need to have them more regularly. It is also important to check with a medical professional if between tests you have any unusual symptoms such as:
*Please note that these symptoms are very general and may not indicate cervical cancer.
The results of your Cervical Screening Test will usually be available within two weeks. You can either schedule a follow up appointment or call your health professional for the results. Your results will also be automatically sent to the National Cancer Screening Register that keeps a record of your screening history and contact you by post if you are overdue for your next test. If you do not wish for this to occur speak to your provider when you have your Cervical Screening Test. You can find out what different results mean at Understanding your Cervical Screening Test results.
It is important to see a health professional regarding specific health needs such as information on pregnancy, early sexual intercourse, sexual abuse, immunodeficiency, and DES exposure.
All women and people with a cervix commence cervical screening at 25 years of age. This starting point for cervical screening has been decided upon after years of research that has found:
Medicare does not cover routine cervical screening for women and people with a cervix under 25 years of age but if you are experiencing symptoms such as unusual bleeding, unusual discharge and pain, please make an appointment with your healthcare provider immediately.
For more information, please visit www.cancerscreening.gov.au/cervical or discuss with your GP what these changes mean for you.
Cervical Screening Tests are recommended every 5 years from the age of 25-74, unless your doctor advises otherwise. If you are 70 years or over and have had regular Cervical Screening Tests, you will be recommended to have an exit HPV Test, but you can continue to undertake cervical screening if you would like to. If you are over 70 years old and have never had a Cervical Screening Test, you can make an appointment to be screened.
There are some rare neuroendocrine cervical cancers that are not caused by HPV. This means they won’t be detected through routine cervical screening tests.
The current HPV vaccine provides protection against about 90% of cervical cancers so it is important that even if you are vaccinated, you are also screened for cervical cancer as you do not have 100% protection.
Cervical cancer affects lesbian, bisexual, queer and pansexual women. Cervical cancer also affects transmen and non-binary people with a cervix. The National Cervical Screening Program (NCSP) in Australia is available to all people with a cervix between the ages of 25 and 74 who have ever been sexually active. Here we look to address any queries about cervical screening for the LGBTQI community.
ACON‘s Cervical Screening campaign, Own It, empowers all women and people with a cervix to own their Cervical Screening Test. See the video about ACON’s campaign.
Human papillomavirus (HPV), the virus that causes almost all cervical cancers, can be transmitted by any kind of sexual contact. Transmission does not require a penis or penetrative sex to be involved. Transmission can occur no matter how you identify. As HPV has no symptoms and tests are not conducted on people with a cervix until they are 25 years old, there is always the possibility that a sexual partner could have contracted the virus and passed it on to you without your or their knowledge. HPV is very common so even if you have only had one sexual partner, you need to be screened.
It is important that you find a medical professional who you feel comfortable with to discuss your cervical screening and other health needs. Your friends may have suggestions, or the following links can help you find a provider in your area.
The Australian Lesbian Medical Association (ALMA) compiles an up to date list of doctors and mental health professionals who are recommended by lesbian and bisexual women.
The Gender Affirming Doctor List from ACON’s TransHub website provides information for trans and gender diverse people in NSW.
The Australian Professional Association for Trans Health (AusPATH), is Australia’s peak body for professionals involved in the health, rights and well-being of trans, gender diverse and non-binary people. They provide a list of health service providers.
By law, health professionals must maintain privacy and confidentiality. If you are happy for your records to be shared with other health professionals, they can be added to your profile with My Health Record.
If you are feeling uncomfortable during the screening process, you can ask to stop or pause the procedure. You can ask any questions that may overcome this discomfort and enable the screening to continue, or you can leave at any time you wish.
You can take a support person with you to your screening appointment. Discuss your concerns about the screening and how they can best support you. Taking a list of questions with you to the appointment can help you check all your concerns have been addressed.
A person cannot be discriminated against due to their gender identity, sexual orientation or lawful sexual activity (Equal Opportunity Act 2010). If you feel discriminated against, sexually harassed, victimised or vilified, you or someone on your behalf can make a complaint to the Human Rights Commission. Discussion with a friend or support person can be helpful if you do not wish to make a complaint.